Thoughts on the Bispectral Index
The Bispectral Index (BIS) is intended to be a dimensionless measure of anaesthetic depth derived from spectral analysis of a frontal electroencephalogram (EEG) in patients undergoing anaesthesia involving neuromuscular block. The minimum value is 0 (isoelectric EEG) and the maximum is 100 (fully awake). BIS of 40-60 is considered adequately deep for general anaesthesia.
BIS is synthesised from frontal EEG data using an undisclosed proprietary algorithm. Morimoto and colleagues (2004) shed some light on the derivation of BIS by analysing its correlation with published formulae for the constituent analyses that are integrated into the final BIS value. In brief, the frontal EEG is processed to remove artefacts and noise, and then a fast Fourier transform is applied to facilitate analysis with respect to time of its constituent wave patterns. The relative prevalence of beta waves (which are dominant in light planes of anaesthesia) constitute the BetaRatio. The degree of synchronicity between fast (40–47 Hz) and slow (0.5–47 Hz) wave patterns is termed SynchFastSlow. This is achieved by the titular bispectral analysis, where greater synchronicity is thought to indicate deeper planes of anaesthesia. These data are combined, likely with other undisclosed analyses, via a propriety formula to report a single BIS value.
The BIS monitor produces two other numbers of clinical relevance: the signal quality index (SQI), the derivation of which is unknown, and the suppression ratio (SR) which indicates the proportion of the preceding minute that the EEG has been in burst suppression. The BIS processing time introduces a delay of approximately 45 seconds from scalp to monitor.
My Experience
I have seen BIS used to measure “depth of anaesthesia” in patients receiving both total intravenous anaesthesia (TIVA) and inhaled volatile anaesthesia, with and without neuromuscular blockade. The invention of BIS has been cited as a boon for proponents of TIVA because it provides “effect site monitoring” analogous to end tidal anaesthetic concentrations (ETAC) used for monitoring inhaled volatile anaesthesia. I have seen BIS used in both critically unwell and very young patients.
Evidence Base
BIS monitoring has been studied as a tool for reducing the incidence of awareness during general anaesthesia with neuromuscular blockade. This effect was evaluated in the landmark B-Aware trial, funded by Aspect Medical Systems (the then-proprietors of BIS).
The B-Aware trial measured the incidence of awareness in 2463 adult patients undergoing general anaesthesia found an absolute risk reduction of 0.74% with a number needed to treat (NNT) of 138. A statistically satisfactory reduction in awareness was achieved. The investigators in the B-Aware trial did not examine the sensitivity or accuracy of BIS as a monitor of anaesthetic depth, and their findings only supported titrating anaesthesia to BIS of 40-60 as a technique to reduce the incidence of awareness.
Shortcomings
Subsequent large-scale studies of BIS have not supported the findings of the B-Aware trial.
The humorously-titled B-Unaware trial from Adivan and colleagues (2008) found that in 2000 patients undergoing general anaesthesia, use of BIS monitoring was not superior to ETAC monitoring for prevention of awareness. The also refuted earlier claims from the B-Aware trial that titrating anaesthetic dose using BIS monitoring was associated with lower utilisation of volatile anaesthetic.
The subsequent BAG-RECALL trial from Adivan and colleagues (2011) expanded on the B-Unaware trial with a substantially larger study group and an international multi-centre implementation. Investigators compared BIS-guided anaesthesia with ETAC-guided anaesthesia in 6041 patients and found that BIS was not superior to ETAC for reducing incidence of awareness. In their findings, BIS was actually associated with a higher rate (0.66%) of awareness than ETAC-guided anaesthesia (0.28%).
When using inhaled volatile anaesthetic, BIS does not correlate with ETAC.
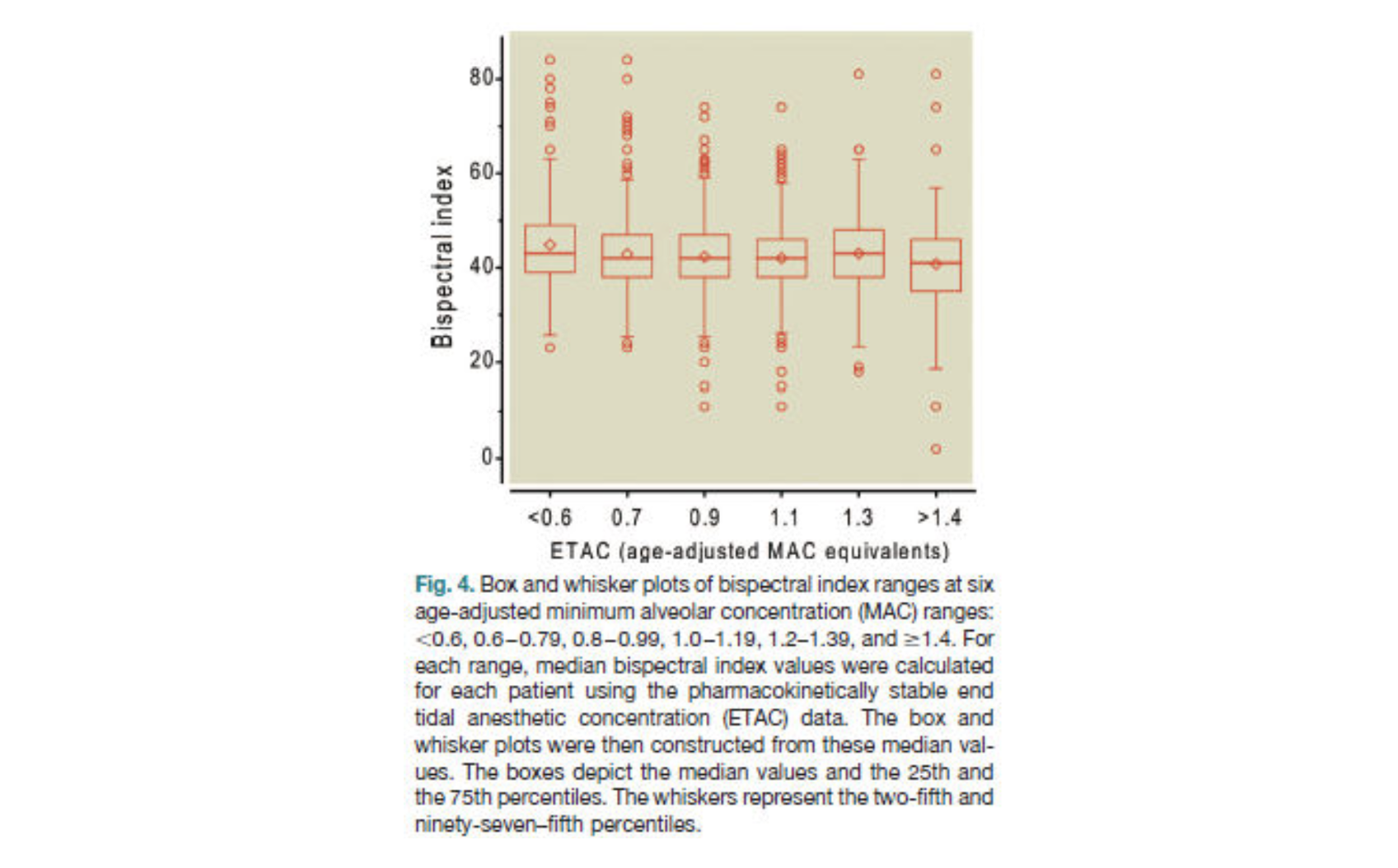
In a post-hoc analysis of data from the B-Unaware trial, Whitlock and colleagues (2011) found that BIS monitoring was clinically insensitive to significant changes in ETAC and was vulnerable to significant inter-individual variability. The following box and whisker plot summarises the insensitivity of BIS to fine titration of volatile anaesthetic.
BIS is vulnerable to interference from EMG data.
Schuller and colleagues (2015) demonstrated the misleading response of BIS to neuromuscular blockade in ten volunteer anaesthetists who received neuromuscular blockade while remaining awake and aware. Though subjects were cognitively unaffected and able to recall all events during the period of paralysis, their respective BIS readings consistently fell into the range suggestive of fully adequate anaesthesia. The following plot of one participant’s BIS values illustrate this effect.
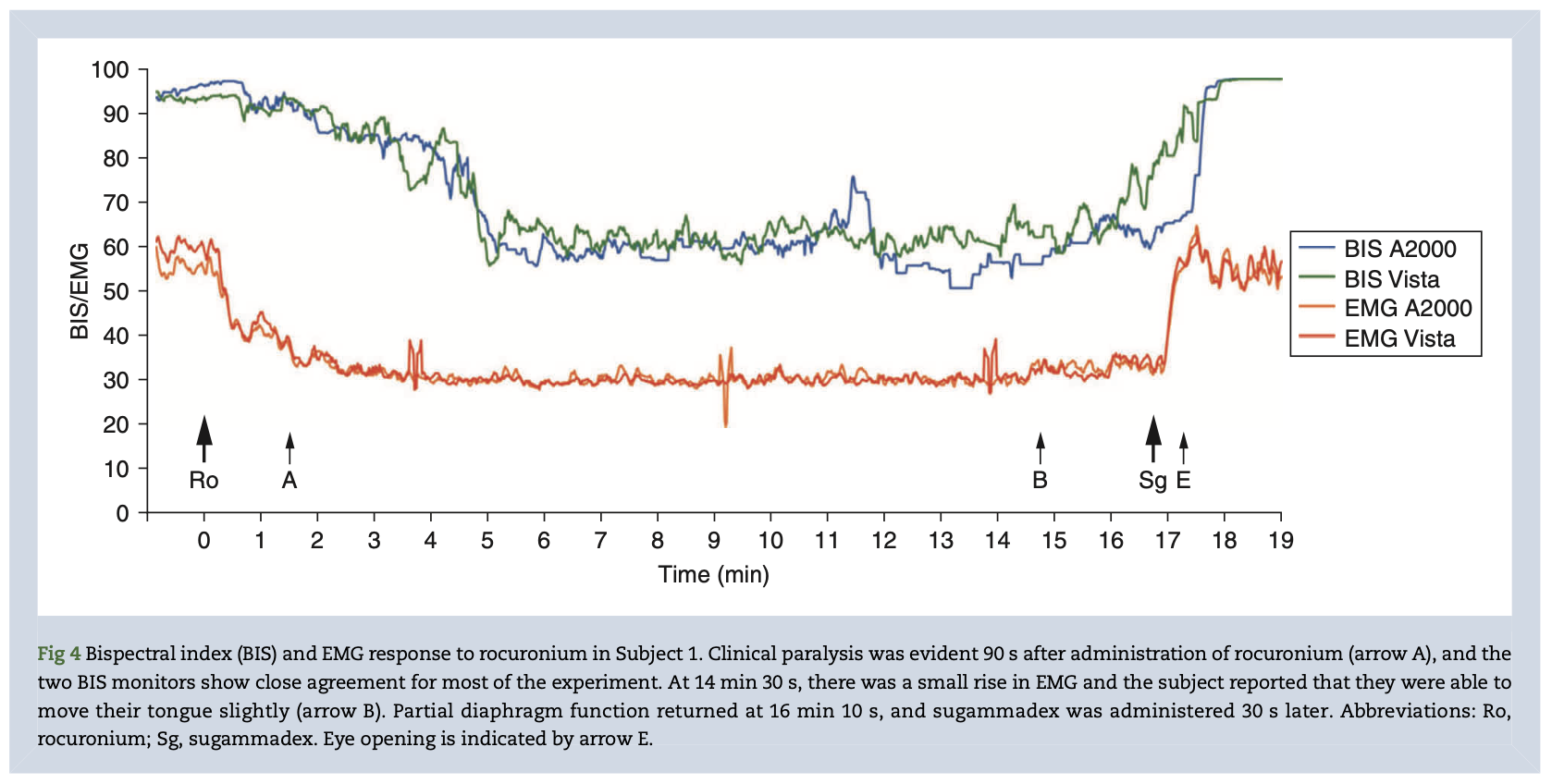
This finding should be particularly interesting in light of the common practice of lightening anaesthesia and letting BIS “drift up” towards the end of a case. This practice may unintentionally introduce a serious risk of awareness, especially given that neuromuscular blockade achieved with rocuronium or vecuronium is commonly maintained until very shortly before emergence thanks to the wide availability and rapid action of sugammadex.
Final Thoughts
To my eye, BIS is too good to be true. How could a device created with twenty year old signal processing technology successfully (let alone reliably) interpret an EEG in the face of copious interference from muscle activity, diathermy probes, and the rest? When I consider the frequent and alarmingly wild misdiagnoses produced by automatic ECG interpretation, BIS seemed like a stretch.
The results of my brief dive into the murky world of signal analysis and the clinical evidence for BIS suggests that my skepticism was at least partly warranted.
References
- Avidan MS, Searleman AC, Bottros M. Anesthesia Awareness and the Bispectral Index. N Engl J Med. 2008;12. PubMed
- Myles P, Leslie K, McNeil J, Forbes A, Chan M. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. The Lancet. 2004 May;363(9423):1757–63. PubMed
- Avidan MS, Jacobsohn E, Glick D, Burnside BA, Zhang L, Villafranca A, et al. Prevention of Intraoperative Awareness in a High-Risk Surgical Population. N Engl J Med. 2011 Aug 18;365(7):591–600. PubMed
- Whitlock EL, Villafranca AJ, Lin N, Palanca BJ, Jacobsohn E, Finkel KJ, et al. Relationship between Bispectral Index Values and Volatile Anesthetic Concentrations during the Maintenance Phase of Anesthesia in the B-Unaware Trial. Anesthesiology. 2011 Dec 1;115(6):1209–18. PubMed
- Schuller PJ, Newell S, Strickland PA, Barry JJ. Response of bispectral index to neuromuscular block in awake volunteers. British Journal of Anaesthesia. 2015 Jul;115:i95–103. PubMed
- Morimoto Y, Hagihira S, Koizumi Y, Ishida K, Matsumoto M, Sakabe T. The Relationship Between Bispectral Index and Electroencephalographic Parameters During Isoflurane Anesthesia: Anesthesia & Analgesia. 2004 May;1336–40. PubMed